Prostate Cancer Detection
PSA – Measurable by Standard Blood Test
As well as producing seminal fluid, the prostate generates a molecule known as prostate-specific antigen, or PSA. Once prostate cancer is diagnosed, monitoring the PSA value is used to monitor the progress of the disease. Depending on the stage of the disease and the treatment used, your doctor’s interpretation of the PSA test will not be based on the same criteria. PSA tests are often recommended from the age of 50 years. The rate of PSA increases in case of a prostate disease but does not allow to diagnose a cancer. For this purpose, additional examinations must be carried out.
Digital Rectal Examination
This examination is performed by a general practitioner during a normal consultation. The physician inserts a finger into the patient’s rectum in order to feel the prostate. This is a quick, painless procedure.
Prostate Biopsies
To determine whether a patient is suffering from prostate cancer, a biopsy is performed. This involves removing tiny fragments of prostate that are then analysed in the laboratory in order to study the types of cell contained in the samples. Before examination is performed, patient is given an enema (washing out the rectum with a liquid solution) and an antibiotic treatment. Under local anesthesia, guided by an ultrasound scanner (with a probe inserted into the rectum) that produces an image of the prostate, the physician collects at least 12 tissue fragments from different parts of the prostate. They are then examined under the microscope by an anatomopathologist who will confirm or not the presence of a cancer. Its objectives are:
- Specify aggressiveness of the cancer cells defined according to a scale called Gleason score (degree of differentiation of the tumor, ie the tendency of the tumor to resemble a normal tissue of the prostate),
- Evaluate number and distribution of positive biopsies (showing cancer cells), characteristics of the tumor tissue and the crossing of the cancer cells beyond the prostate capsule.
Gleason Score
The Gleason score is determined after analyzing prostate biopsies. There are five types of prostate cell: type 1 cells are normal and type 5 are those in which cancer is the most advanced. The Gleason score is calculated by observing which of the cell types in the specimen are most numerous and adding them together. The score ranges from 6 to 10, depending on the aggressiveness of the cancer, with 10 being the most aggressive form.
Degree of risk or aggressiveness, based on the Gleason score:
- 6 or 7: low or intermediate-risk cancer
- Between 8 and 10: high-risk cancer
The Gleason score is generally expressed as follows: Gleason 7 (3+4). Concerning the figures in brackets, the first digit indicates the most numerous cell type in the biopsy specimens and the second digit is the second most numerous cell type.
Staging
When prostate cancer has been diagnosed, the diagnosis must be refined by performing a series of imaging examinations for the staging assessment. The purpose of the staging assessment is to accurately determine whether the cancer is localized (i.e. wholly contained within the prostate gland) or has spread.
Scan
This painless examination, which lasts between 10 and 15 minutes, uses X-rays to produce a very accurate image of the target area, in this case the abdomen and groin (abdominopelvic scan). The scan will reveal whether the prostate cancer has remained within the gland or has instead reached the prostatic capsule (i.e. the membrane surrounding the prostate), the lymph nodes.
Magnetic Resonance Imaging (MRI)
An MRI scan is similar to an X-ray scan except that it uses a magnetic field rather than rays. This examination provides a very accurate image of the body’s soft tissue, allowing the physician to see whether the cancer has spread to any other organs.
Bone Scintigraphy (bone scan)
This examination reveals whether a prostate cancer has reached the skeleton. Bone scintigraphy is a painless procedure in which a product is injected into the blood in order to reveal any bony metastases on the images subsequently produced.
Prostate Cancer Different Stages
The type of treatment prescribed for cancer is largely determined by the disease’s stage of development. The following scale indicates the degree of progression of the prostate cancer, from least-advanced to most-advanced:
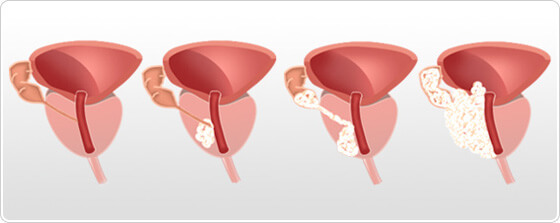
Prostate cancer stages T1, T2, T3, T4
Localized Cancers:
- Stage T1: corresponds to a tumor not detectable by a digital rectal examination. Only a few cells are cancerous. The patient does not experience any symptoms of the disease.
- Stage T2: corresponds to a cancer that is detectable by a digital rectal examination (a hard lump can be felt) and appears to be fully contained within the gland, whether in both lobes of the prostate or just one.
Advanced Cancers:
- Stage T3: corresponds to a cancer that extends beyond the prostate and/or seminal vesicles.
- Stage T4: corresponds to a cancer that has spread to other organs near the prostate (such as the bladder and/or rectum).
